Mechanical low back pain is one of the most common reasons patients seek medical care. Approximately two out of three adults are affected by mechanical low back pain at some point in their lives. Low back pain affects men and women equally. The onset most frequently occurs in people aged 30-50 years. Low back pain is the most common and most expensive cause of work-related disability in the United States. Smokers appear to have an increased incidence of back pain compared with nonsmokers. Furthermore, the incidence of current smoking and the association with low back pain is higher in adolescents than in adults.
Many causes of mechanical low back pain exist. The most common causes are age related degenerative conditions such as disc degeneration, facet arthropathy and muscle ligament injuries. Sciatica or radicular pain can arise from nerve root impingement due to herniated discs. This pain tends to be sharp, well localized, and can be associated with numbness, tingling and weakness. At times, pain from nerve irritation can be dull, poorly localized, and without numbness or tingling.
The cause of impingement syndrome is most commonly herniated discs, but it may also be caused by spinal stenosis, spinal degeneration, or cauda equina syndrome.
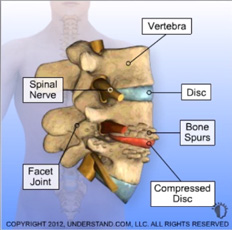
Herniated discs are produced as spinal discs degenerate. After growing thinner, the nucleus pulposus herniates out of the central cavity against a nerve root. Intervertebral discs begin to degenerate by the third decade of life, and herniated discs are found on autopsy in one third of adults older than 20 years. Only 3% of these, however, are symptomatic. The most common locations for herniation are L4, L5, and S1.
Spinal stenosis occurs when disc spaces decrease as intervertebral discs lose moisture and volume with age. Even minor trauma under these ircumstances can cause inflammation or nerve root impingement, which can produce classic sciatica pain without disc rupture. The pain can often be bilateral.
Spinal degeneration is caused by alterations in the hygroscopic quality of the nucleus pulposus. This process progresses to annular degeneration. Coupled with progressive posterior facet disease, this process leads to spinal canal or foraminal encroachment. These retrogressive and proliferative changes in the disc anteriorly and the joints posteriorly produce clinical symptoms and radiographic findings termed 3-joint complex degeneration.
Cauda equina syndrome is produced by massive midline extrusion of nuclear material or tumor into the spinal canal, which compresses the caudal sac. The classic presentation is bilateral sciatica, with lower extremity bowel or bladder dysfunction present in 90% of patients. Urinary retention is initially observed and followed by overflow incontinence. Perineal or perianal anesthesia is present in 60-80% of patients.
Musculoskeletal pain syndromes that produce low back pain include myofascial pain syndromes and fibromyalgia. Myofascial pain is characterized by pain and tenderness over localized areas (trigger points), loss of range of motion in the involved muscle groups, and pain radiating in a characteristic distribution but restricted to a peripheral nerve. Relief of pain is often reported when the involved muscle group is stretched. Fibromyalgia results in pain and tenderness on palpation of 11 of 18 trigger points, one of which is the low back area, as classified by the American College of Rheumatology. Generalized stiffness, fatigue, and muscle ache are reported.
Other skeletal causes of low back pain include osteomyelitis, sacroiliitis, and malignancy. Osteomyelitis results from infectious processes involving the bones of the spine, while sacroiliitis results from inflammatory changes in the sacroiliac joints. This pain presents over the sacroiliac joints and radiates to the anterior and posterior thighs. This pain is usually worse at night and is exacerbated by prolonged sitting or standing. Malignant tumors of the spine can be primary or metastatic. Most primary spinal tumors are found in patients younger than 30 years and usually involve the posterior vertebral elements. Metastatic tumors are found mostly in patients older than 50 years and tend to occur in the anterior aspects of the vertebral body.[9] Caution is advised, in that these traditional “red flags” have sufficient evidence in detecting spinalmalignancy if based on the presence of a single red flag. However, the presence of more than 2 of these together should increase suspicion for the need for further workup.

Dr. Ram R. Vasudevan, MD, FAANS
Austin NeuroSpine PLLC
5300 Bee Cave Road, Building 1,
Suite 220 Austin, TX 78746
Phone: (512) 640-0010
Monday: 8:00 AM – 5:00 PM
Tuesday: 8:00 AM – 5:00 PM
Wednesday: 8:00 AM – 5:00 PM
Thursday: 8:00 AM – 5:00 PM
Friday: 8:00 AM – 5:00 PM
Saturday: Closed
Sunday: Closed
© 2023 Austin NeuroSpine PLLC. All rights reserved.